Brugada Syndrome, One Of The Main Causes Of Sudden Death
Brugada syndrome is one of the leading causes of sudden death in the world, but it has not been long since it has been discovered. It was described in 1992 by two brothers named Brugada.
The disorder is genetic and consists of an alteration of the electrical transmission system of the heart. In any case, the symptoms do not become evident until adulthood, and there are no previous signs that allow us to suspect it.
The genetic defect in question alters the ion channels of the myocardium, which is the muscle tissue of the heart. Ion channels allow the exchange of positive and negative charges between the interior and exterior of myocardial cells. When it fails, the person is more prone to ventricular fibrillation.
Ventricular fibrillations are serious arrhythmias. The heart beats uncontrollably at a very high speed, up to more than 200 or 300 beats per minute. It is a fatal arrhythmia if not addressed in time.
Signs and symptoms of Brugada syndrome
We already anticipated that Brugada syndrome does not have specific symptoms. It is difficult to diagnose and detect because it does not present previous alterations that warn of the existence of the alteration of the ionic channels.
When the syndrome debuts in an adult individual, it directly presents itself with a certain severity. Syncope, fainting, arrhythmia with palpitations, or cardiac arrest may occur.
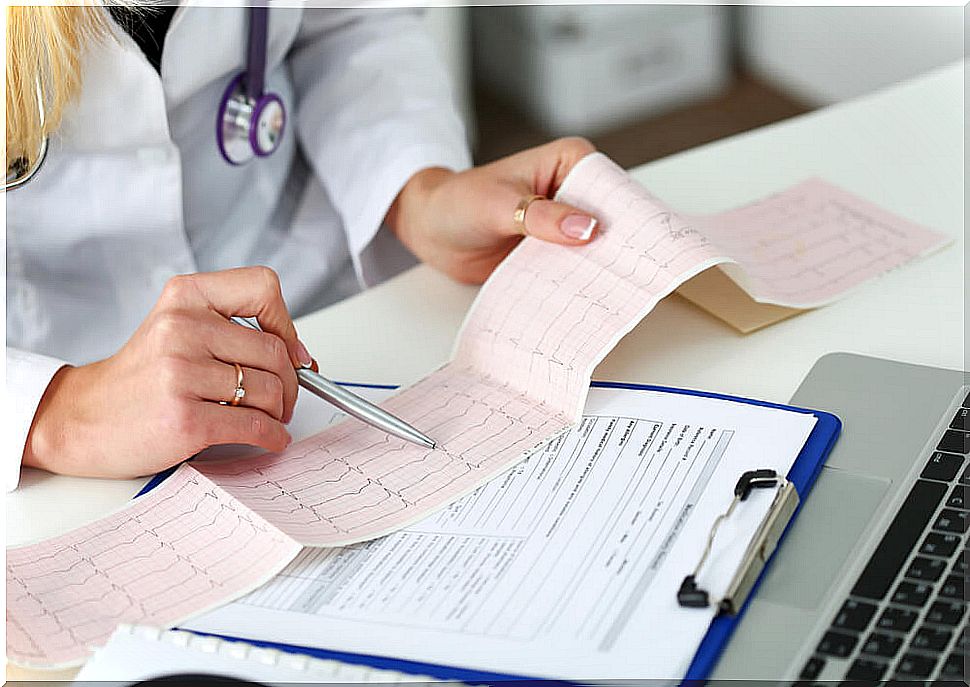
Once the first episode is established, it will be the doctor who will be responsible for suspecting the existence of this syndrome. To do this, you must practice a series of electrocardiograms looking for something known as the Brugada sign, which we will explain later.
This sign only appears on an electrocardiogram and cannot be felt by the patient. Although it is almost impossible to suspect in advance, there are some risk factors that can be taken into account to refine the diagnosis. Among these factors we have:
- Relatives with Brugada syndrome: being a genetic disease, it should be suspected in families that already have it diagnosed.
- Men: the disease is much more common in men than in women.
- Asians: People of Asian descent are more likely to suffer from it.
Diagnosis
Arriving at the diagnosis of Brugada syndrome is a challenge for any physician. In addition to suspecting it, you must have enough persistence to reliably detect it in a test.
The study of choice is the electrocardiogram. It is an electrical recording of cardiac activity that can be performed in an office on an outpatient basis. Through this test, the Brugada sign is searched, a particular form of the study tracing that warns of the presence of alteration in ion channels.
The problem, too, is that not all patients show it on the electrocardiogram, and not all electrocardiograms always record it. The Brugada sign is an elevation of a segment of the path that is very striking.
The other study that may be indicated is the electrophysiological one. It is no longer a complementary method that can be done in an office setting. An operating room is required to insert a catheter into the body. The catheter is brought into the heart to record the organ’s activity from within.
Can it be treated?
It is difficult to talk about a treatment for Brugada syndrome. Strictly speaking, there is no way to get rid of the condition permanently. What does exist is a preventive modality for cardiac arrest.
This prevention is carried out with the implantation of an implantable defibrillator in the patient’s body. This small device records the electrical activity of the heart and acts with an electric shock if it detects ventricular fibrillation.
There are no medications for the syndrome, and there are no surgeries that can be performed to remove defective areas of the heart. Therefore, regular checks are essential.
Living with Brugada syndrome
It is possible to live a long time with Brugada syndrome. Beyond the implantation of a defibrillator or not, the fundamental thing is the controls.
Once the disorder has been detected, it is necessary to follow-up by specialized cardiologists who review the variables to alert about changes.
Similarly, the patient must learn to control risk factors that could increase their risk of cardiac arrest.